Jump to: Eat a whole-food lower-carb diet to lower insulin resistance | Make sure you’re eating enough | Boost intake of calcium, iron, magnesium, and B vitamins | Take home message
Determining what to eat during your menstrual cycle should focus on:
- Eating a diet that helps you achieve good health and balance your hormones throughout your cycle.
- Increasing your intake of specific foods or supplements that may alleviate menstrual discomfort.
Eating a lower-carb diet based on whole foods can help you achieve good all-around health as it’s been shown to impact hormonal balance in women positively.
Research suggests lower-carb diets improve insulin resistance, which can lead to the excess production of androgens, like testosterone.
Within a lower-carb diet based on whole foods, we must also ensure you eat enough. Research has shown that strict dieting and low-calorie diets can interrupt the menstrual cycle and lead to menstrual abnormalities.
There also seems to be a connection between diet and menstrual pain, primarily driven by the increased levels of compounds in the body known as prostaglandins.
Foods rich in B vitamins, such as green leafy vegetables and liver, have been associated with lower levels of discomfort during menstruation.
Consuming more iron and omega-3s may also improve symptoms such as pain and reduce intensive bleeding.

The menstrual cycle phases
The menstrual cycle starts on the first day of your period and again when the next period begins. This cycle typically lasts between 24 and 38 days. During this cycle, there’s a host of changes in the balance of hormones to prepare for pregnancy.
It occurs over four stages:
1) Menses phase
2) Follicular phase
3) Ovulation (ovulation)
4) Luteal phase
Hormonal changes during these phases are ongoing, sometimes unpredictable, and very individual; it’s challenging to know exactly what to eat (and when) to optimise your body’s response as you go through the different cycle stages.
You may have heard of proponents online advocating for a diet optimised to the different phases of your menstrual cycle, often referred to as ‘cycle syncing’.
As of yet, there’s no scientific evidence that this approach is effective at improving your health, hormonal balance, or fertility in the long term – compared to eating a healthy balanced diet with more flexibility.
It may also add more stress (to an already potentially stressful experience) by focusing too rigidly on what you ‘should’ and ‘shouldn’t’ be eating over your menstrual cycle. Generally, achieving good health will get you where you want to be.
During your period or pre-menstrual cycle, you might also experience pain, low energy levels, cramps, bloating, fatigue, and even depression or mood swings (pre-menstrual symptoms, PMS) due to the balance of hormone levels changing as your body prepares you for pregnancy.
Research has suggested that around 88% of women experience menstrual pain and discomfort, which can lead to cravings for rich foods to try and soothe the discomfort.
At Second Nature, you receive 1-2-1 support from a registered dietitian or nutritionist who can guide you through your cycle to ensure you optimise your health for your personal situation and preferences.
Join over 150,000 people like Carla, who’ve joined Second Nature and hopes that our holistic approach will help to improve her hormone balance after seeing improvements in her hormonal health and well-being.
Click here to take our health quiz.
Otherwise, keep reading as we dive into the three areas of research exploring the role of nutrition and the menstrual cycle.
1) Eat a whole-food lower-carb diet to lower insulin resistance
Insulin is an essential hormone in your body that plays a critical role in your metabolism; it also seems to have a role in maintaining a healthy balance of sex hormones.
Insulin resistance is when your body’s cells no longer respond to insulin and its functions.
Research has suggested that insulin resistance can increase by around 15% between the menses and the luteal phases of your cycle.
This rise in insulin resistance is closely associated with the sex hormones estradiol (an estrogen), FSH, and SHGB.
Insulin resistance can also lead to the excess production of androgens like testosterone, which can disrupt the menstrual cycle and is implicated in the development of PCOS.
Therefore, having a low level of insulin resistance might help to ensure your sex hormones are in a healthy balance throughout your cycle and that the cyclic rise observed between the menses and luteal phases doesn’t lead to complications in the long term.
Lower-carb diets based on whole food have been shown to lower insulin resistance, manage blood sugar levels, and support the hormonal balance of crucial sex hormones regulating the menstrual cycle.
When we say lower-carb, we don’t mean ‘no-carb’ – but lower than a standard Western diet rich in ultra-processed foods, refined carbohydrates, and sugars.
A clinical study compared the effect of a lower-carb diet (around 41% of energy from carbohydrates) to a standard high-carbohydrate diet (around 55% of energy from carbohydrates) on markers of insulin resistance and reproductive hormones such as testosterone.
Both groups lost a small amount of weight (1.3kg & 1.66kg) and saw improvements in insulin resistance.
Interestingly, the lower-carb group was almost twice as effective at lowering insulin resistance and decreased testosterone levels by 24.5%. Compared to the high-carb diet, which did not affect testosterone levels.
Similarly, a meta-analysis (a study comparing many studies on the same topic) looking at the impact of lower-carb diets on women living with PCOS found a positive effect of lower-carb diets on insulin resistance and testosterone compared to low-fat diets. Particularly those lasting more than four weeks.
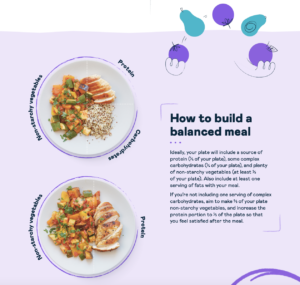
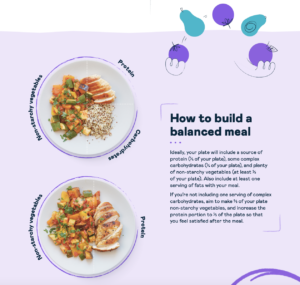
Lower-carb diets encourage the consumption of:
- High-fibre complex carbohydrates like whole grains, sweet potato, quinoa, lentils, and brown rice.
- Healthy fats like avocado, pumpkin seeds, nuts, extra virgin olive oil, dairy, and fat from meat and fish.
- Protein like meat, fish, eggs, tofu, tempeh, and dairy.
- A high intake of non-starchy vegetables like dark leafy greens, broccoli, sauerkraut, and peppers.
- Low-sugar foods like dark chocolate.
Key points:
- Insulin is a crucial hormone involved in metabolism and sex hormone balance.
- Insulin resistance can lead to excess testosterone production and is linked to conditions like PCOS.
- Insulin resistance rises as you progress through the four phases of the menstrual cycle.Lowering insulin resistance through a lower-carb diet based on whole foods can help to ensure a healthy balance of sex hormones.
2) Make sure you’re eating enough
During strict crash diets low in total calories (energy), the body goes into a phase known as metabolic adaptation.
The brain senses the lack of incoming energy, instructs the body to conserve energy at all costs, and prioritises the most critical organs, primarily the brain, heart, liver, and kidneys.
This often means that our reproductive system is de-prioritised and the production of hormones essential in regulating the menstrual cycle is lower, negatively impacting the whole system.
This was demonstrated in a clinical study where 22 women were placed on an 800-1200 kcal diet for their individual menstrual cycles (between 24-38 days). The results indicated a significant drop in the sex hormones regulating the menstrual cycle and fertility.
For example, FSH (follicle-stimulating hormone, essential in maintaining the production and growth of ovarian follicles) dropped by 13.5% and LH (luteinizing hormone, necessary in the release of the egg and production of progesterone) by 38.5%.
These changes were outside the typical transient changes observed in these hormones during a regular cycle, where energy availability is higher.
Fortunately, resuming your regular eating habits and ensuring you’re eating enough total energy can return your hormone balance to normal.
A randomised controlled trial was conducted in exercising women with abnormal menstruation (amenorrhoea or oligomenorrhea).
The participants were split into two groups, one group would be instructed to increase their energy intake by 20-40%, and the other would continue their eating habits.
The study showed that after 12 months, women who increased their energy intake were 45% more likely to have their menstrual function return to normal and see their progesterone levels and estrogen levels normalise.
How can you ensure you’re eating enough?
- Eat until you’re comfortably full: find our hunger scale here.
- Include healthy snacks between meals if you need to: find some ideas here.
- Avoid restricting whole food groups: find an NHS-trusted meal plan here.
Key points:
- Strict dieting and calorie restriction leads to decreased metabolism and prioritising energy for essential organs such as the liver and brain.
- Reproductive systems are often left short of energy, negatively impacting their function.
- Research in women has shown this can significantly decrease essential sex hormones regulating the menstrual cycle.
- However, research has shown that the resumption of a higher energy intake can help menstrual cycles return to normal.
3) Boost your intake of iron, B vitamins, and omega-3s
Iron
Heavy menstrual bleeding is common in women of reproductive age and can contribute to iron deficiency and anaemia.
Iron deficiency can lead to lethargy, heart palpitations, and trouble breathing. It can significantly impact your quality of life and make menstruation even more challenging.
Because of this, increasing your iron intake during your period and ensuring a healthy level of iron intake in your regular diet can help you avoid iron deficiency and the added complications it brings.
Research also suggests that increased iron intake may help lower your risk of experiencing menstrual pain and heavy bleeding. A cross-sectional study of women in Spain supported this.
The study showed that women with a higher intake of iron through animal products such as red meat and pork – had fewer days of intensive bleeding and subsequently had less blood loss.
Another study showed a similar relationship between high intakes of non-haem iron from plant-based sources.
B vitamins
B vitamins, particularly folate (or folic acid), play an important role in what’s known as the ‘one-carbon cycle’.
The one-carbon cycle is the process by which the body produces antioxidants to maintain a healthy balance of oxidative stress within the body’s cells, particularly those in our reproductive system.
Keeping levels of oxidative stress low may help regulate your menstrual cycle. Observational research has consistently shown positive associations between B vitamin intake, fertility, and a lower risk of experiencing symptoms like pain during menstruation.
However, as this research is observational – it isn’t easy to know whether the B vitamins had this positive effect or other elements in their lifestyle.
Still, there’s good evidence that B vitamins play a crucial role in keeping oxidative stress down, which seems to improve reproductive function.
Omega-3 fatty acids: EPA/DHA
Omega-3s (EPA/DHA) are poly-unsaturated fats found in oily fish and algae, and can be converted from the plant-based omega-3 ALA, but only in small amounts.
Omega-3s are a potent anti-inflammatory and may help to lower the discomfort associated with menstruation.
This was supported by a clinical trial in 78 women who experienced menstrual cramps and pain.
The study showed a significant reduction in cramps and overall menstrual discomfort after 3-4 months (depending on individual menstrual cycle length) of taking fish oil tablets.
Interestingly, the most significant reduction in menstrual discomfort was seen in women taking fish oil and B12 supplementation.
How to boost iron, B vitamins, and omega-3s EPA/DHA
Iron-rich foods: Meat, fish, seafood, dark leafy greens, legumes, or supplementation. (Consume plant-based sources of iron with vitamin C-containing foods such as peppers and broccoli as this increases absorption.)
B vitamins: Dark leafy greens and veggies, nuts and seeds, salmon, red meat, liver and other organ meats, eggs, dairy, or supplementation.
Omega-3s EPA/DHA: Salmon, trout, other oily fish, algae, supplementation. (You can also consume flaxseed and chia seed to boost ALA intake, which may be converted into EPA or DHA.)
Key points:
- Heavy menstrual bleeding is very common and can lead to iron deficiency and anaemia.
- Observational research suggests women with high iron intakes from both animal (haem) and plant (non-haem) can reduce the risk of having menstrual discomfort and lower the intensity of bleeding.
- B vitamins support your body’s natural antioxidant defences, and increasing your intake of B vitamins is associated with a reduced risk of menstrual discomfort.
- Omega-3s EPA/DHA have also been shown in clinical trials to reduce menstrual discomfort; this effect was enhanced when fish oil tablets were coupled with vitamin B12.
- You can boost your intake of these foods through your diet or supplementation; both are safe and effective.
Take home message
Your hormones will naturally fluctuate throughout your menstrual cycle as your body prepares you for pregnancy.
Due to the individual differences in the release and balance of these hormones, it’s challenging to determine precisely what to eat during which phase.
However, by maintaining your health by lowering insulin resistance, eating enough, and boosting your intake of specific nutrients like omega-3s and B vitamins, you can improve your menstrual cycle rhythm, lower your risk of heavy bleeding, and reduce the severity of menstrual discomfort.