Most of us are familiar with the feeling of nerves and anxiety in our gut. It’s where the phrase ‘butterflies in the stomach’ comes from. Individuals with irritable bowel syndrome (IBS) tend to report stomach flare-ups at times of high emotion. So, our gut clearly influences our emotional state. But is this link bidirectional? Recent research suggests that our gut actually affects our brain and emotions.
Medication-assisted weight loss with a future focus
Start with Mounjaro, transition to habit-based health with our support

A note on the gut
The human gut is an extremely complex system. The large intestine is home to roughly 100 trillion micro-organisms. To put it in context, that’s more bacteria than there have ever been people living on this planet. This community of bacteria is called our gut microbiome. Many factors, diet being a huge one, can affect the population and diversity of our gut microbiome.
Studies on human twins are useful in determining whether something is genetically defined or heavily influenced by the environment, since twins have almost identical DNA but may have grown up separately.
Twin studies suggest that environmental factors, such as diet and drugs, are more significant determinants of the microbiota composition than genetic components.
Key points:
- The human gut is an incredibly complex system.
- It is home to hundreds of billions of bacteria.
Does our diet influence mental health?
The field of science that focuses on the links between diet, gut health, and mental illness is extremely new and mostly limited to animal studies or human observational studies.
One recent clinical intervention trial examined whether diet could improve depressive symptoms in 166 individuals diagnosed with clinical depression undergoing treatment (either medication, therapy, or both).
Half the participants were instructed to follow a Mediterranean style diet (lots of vegetables, fish, whole grains, and healthy fats), while the other half received social support sessions in line with the traditional treatment of depression. The dietary intervention group experienced a more substantial reduction in depressive symptoms over the three months. In addition, significantly more participants in the diet group met the criteria for remission of major depression.
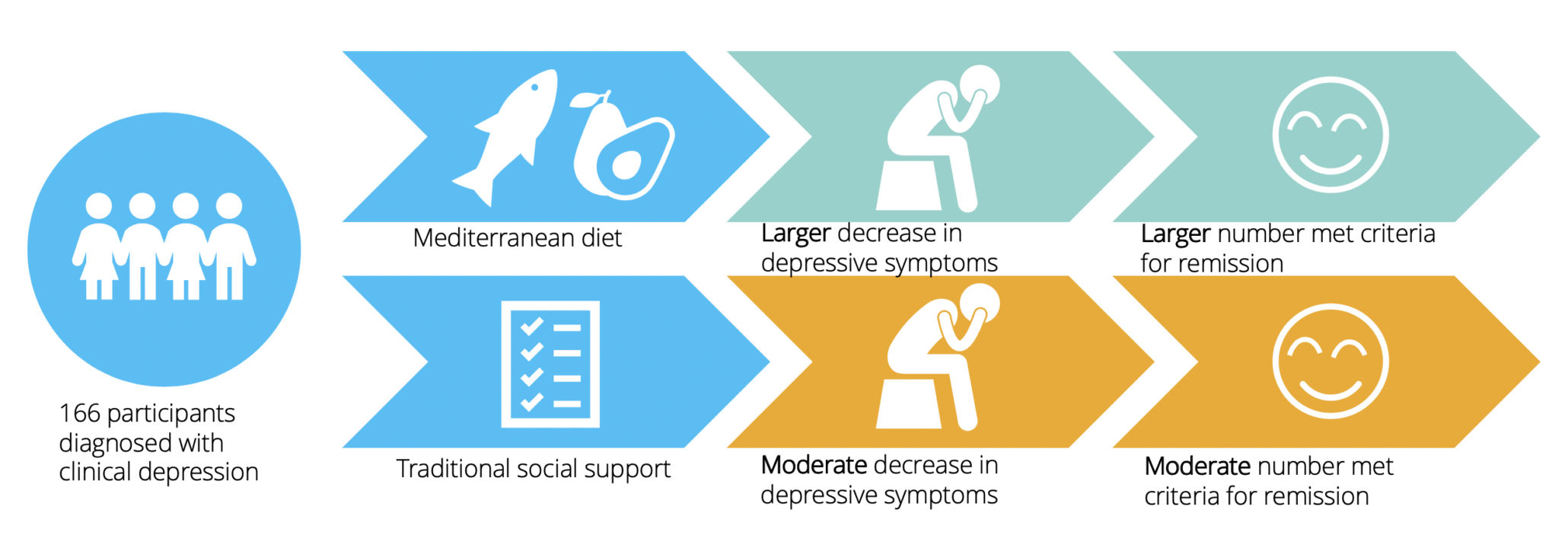
Several potential mechanisms could explain the reduction of depressive symptoms in the dietary intervention group. The effect was independent of weight change, so body composition is not the likely mechanism. The researchers suggest that one potential mechanism by which diet influenced depressive symptoms could be via the gut microbiome.
Supporting this, a review on the topic concluded that the gut microbiota is a crucial mediating factor of mood and emotions in humans.
While the evidence is promising, it’s important to remember that this is a new, emerging field there is not enough evidence yet to prove a direct link between changes in gut microbiota and an improvement in depressive symptoms. It does, however, provide further incentive to follow a healthy, balanced diet, which benefits overall health.
Key points:
- New evidence suggests that our diet can impact our mental health.
- Following a healthy, balanced diet appears to reduce depressive symptoms.
How is our gut linked to our brain?
The suggested mechanism by which diet may interact with our mood is via the gut-brain axis. This axis refers to the signalling that occurs between our gut and our central nervous system (CNS), which comprises the spinal cord and the brain. Gut permeability, which refers to the gut allowing substances to pass through it, is thought to play a role.
When ‘good’ bacteria in our gut is reduced, for example, from antibiotics, ‘bad’ bacteria get a chance to colonise our gut lining. Inflammation occurs in response to the toxins this process produces, which increases gut permeability. When our gut lining is more permeable, specific compounds may be able to gain access to areas within the CNS that regulate our emotions.
Key point:
- The gut-brain axis is the proposed mechanism by which our gut influences our brain.
Pre- and probiotics
Pre- and probiotics both promote gut health by increasing the number and diversity of ‘good’ bacteria in the gut by different mechanisms. Therefore, it’s interesting to explore whether increasing either can impact mental health.
Prebiotics
Prebiotics act as a fertiliser for good bacteria in our guts, promoting their growth. Prebiotics are usually non-digestible plant fibre, found in foods such as artichoke and asparagus. A study with healthy volunteers demonstrated that prebiotic supplementation altered emotional bias towards positive rather than negative stimuli in attention tasks. These results suggest that prebiotics promote ‘good’ gut bacteria and subsequently influences our brain.
You should be getting enough prebiotics by having a variety of plant-based foods, so prebiotic supplements aren’t necessary if you have a balanced, varied diet. Examples of prebiotic foods you can add to your diet include onions, asparagus, artichoke, chicory root, garlic, leeks, wheat bran, oats, apples, and bananas.
Probiotics
Probiotics are the actual good bacteria, of which there are thousands of different strains. They are found in fermented foods and live dairy products, usually called ‘live cultures’.
A commonly referenced study demonstrated that supplementation of a fermented probiotic milk drink for 4 weeks influenced the brain regions that control emotion and sensation in healthy women.
However, a large company that produces and sells fermented dairy drinks funded this study, so these findings must be taken with caution.
Another randomised, placebo-controlled trial, without any conflict of interest, showed that individuals given a probiotic supplement, containing many different species, demonstrated a reduction in cognitive reactivity scores. Cognitive reactivity refers to disturbed patterns of thinking triggered by changes in mood and can be a significant risk factor for depression.
This evidence suggests that ‘good’ bacteria in the gut affects the brain. Further research is needed to determine if it’s the combination of probiotic strains that provide the benefit or whether one particular strain is responsible.
An important point is that there are billions of different types within hundreds of different strains of bacteria. So far, research has focused on roughly only 4 strains. Additionally, gut microbiome individuality means that everyone responds differently to various bacteria, so taking a one-size-fits-all approach to probiotic supplementation is not helpful.
Supporting this, a paper published in the journal Cell noted that different people demonstrate resistance to different probiotics depending on the strain of bacteria, individual microbiome, and area of colonisation.
It also discussed that certain strains of probiotics might compete with each other for colonisation resulting in both strains losing out. The authors highlight that once it is understood how unique gut microbes reject colonisation of specific probiotic strains, we can develop ways to counteract this resistance and implement the beneficial effects of probiotics.
The average healthy person doesn’t need a probiotic supplement to have a healthy gut. Foods that contain live cultures include yoghurt, soft cheese and fermented foods like kimchi, sauerkraut (cabbage), tempeh (fermented soybeans), kombucha, and kefir (fermented milk beverage). Until scientific advances allow individual assessment of which particular strains, or combinations of strains, provide benefits, eating a variety of these foods helps to ensure different species of probiotics are available to our bodies.
The clinical trials discussed suggest a direct effect of pre and probiotics on the brain, supporting the role of gut health in mental health. Animal studies showing that probiotics reduce intestinal permeability and depressive symptoms in rats support the previously proposed mechanism of the gut-brain axis.
Key points:
- Prebiotics act as a fertiliser for good bacteria in our guts, whereas probiotics are the good bacteria.
- Both promote gut health through different mechanisms.
- Preliminary clinical evidence suggests that pre- and probiotics can improve mental health.
- Gut response to probiotics greatly varies between individuals.
- It is not necessary to supplement pre- and probiotics as a healthy, balanced diet high in plant fibre, foods containing ‘live cultures’ and fermented foods is enough.
Take home message
- Our brain is clearly connected to our gut, as many people experience physical gut symptoms when they feel stressed or anxious.
- Environmental factors, such as diet seem to have a significant impact on our gut health.
- Recent research suggests that improving our diet can impact our brains and potentially improve our mental health.
- A potential mechanism for this is an improvement in gut health, but since it is a new area of research more evidence is needed to confirm this.
- Studies exploring the effect of pre- and probiotics on the brain support this theory.
- There is a huge amount of individual variability in the gut microbiome response to different probiotics.
- This research is hugely novel, and there is by no means enough evidence yet to solidify these claims.
- It does provide further incentive though to treat our gut well by eating a balanced diet with a variety of vegetables and little ultra-processed foods.


