Jump to: What does insulin do? | How the body stores fat | How the body burns energy | How carbohydrates influence energy use | Take home message
In our first guide of this series, we discussed the personal fat threshold hypothesis, how to measure it, and how the body regulates fat and carbohydrates to help us understand the process leading to type 2 diabetes and high blood sugar levels.
In this article and part two of the series, we’ll summarise how insulin plays a vital role in regulating energy in the body and, therefore, has a significant effect in determining your personal fat threshold.
Medication-assisted weight loss with a future focus
Start with Mounjaro, transition to habit-based health with our support

What does insulin do?
One of insulin’s prominent roles is transporting excess energy, fat or carbohydrate (glucose), into our fat cells (adipose tissue) to store.
The body’s ability to store excess energy as fat in the adipose tissue is an essential process for ensuring:
- Excess energy doesn’t build up in the cells such as those in the muscles or organs.
- Excess energy doesn’t build up in the bloodstream.
- Fat isn’t stored within the internal organs as visceral fat.
Why’s this important?
If we can understand what influences our body’s ability to store and use the energy we get from food, we can look at strategies to improve these systems and our overall health.
If your weight is currently within the ‘healthy’ range for BMI, and you’re living with type 2 diabetes, then focusing on weight loss alone is unlikely to benefit your health and could pose further health risks such as poor bone health.
However, focusing on interventions that will improve the function of your body’s energy systems will result in improved health while still allowing you to maintain your current weight.
On the other hand, if you’re currently overweight or obese and living with type 2 diabetes, it’s essential to focus on improving the function of your body’s energy systems alongside weight loss, as weight loss alone may not guarantee better management of your type 2 diabetes in the long term.
At Second Nature, we provide you with the support of a registered nutritionist or dietitian who’s trained in the physiology of type 2 diabetes. We can support you in making healthy lifestyle changes to improve your condition.
If you’re currently living with type 2 diabetes and would like to join the Second Nature programme to see if you can lower your blood sugar levels, improve your health, and reduce your reliance on medications, you have two options:
- Speak to your GP to see whether Second Nature is available in your area and whether they can refer you to the programme.
- Click here to take our health quiz and join over 150,000 people who’ve improved their health with Second Nature.
Otherwise, keep reading as we look to improve your understanding of the body’s energy systems. Our focus today will be reviewing the body’s largest pool of stored energy, adipose tissue, and its relationship with insulin.
1) How the body stores fat
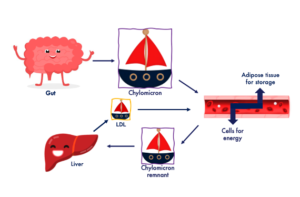
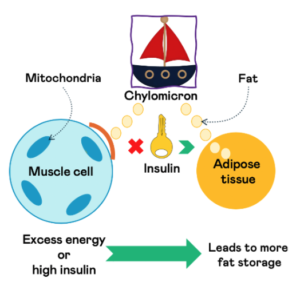
Fat is transported around the body in small boats known as chylomicrons (pronounced ky-low-my-crons). These boats transport fat around the body to either be stored in the adipose tissue or used by the cells for energy.
What happens to fat when it enters the adipose tissue?
The adipose tissue has two ways of storing fat in its cells:
- Fat cells can increase in size; we call this adipose tissue hypertrophy.
- We can form new fat cells from dormant cells that we call pre-adipocytes. This process of forming new fat cells is known as adipose tissue hyperplasia.
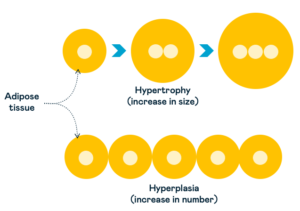
Whether your body can increase the fat cells in size or number will influence your personal fat threshold.
Research has shown that increasing the number of fat cells (hyperplasia) is more beneficial than size (hypertrophy).
2) How the body burns energy
The body’s two primary fuel sources are fat and glucose (carbohydrates). The brain will prioritise using glucose as its energy source because fat can’t be transported directly into the brain.
However, regarding the rest of the body, like our muscles and our internal organs, such as the heart and liver, two key factors determine what fuel the cells will use for energy:
- Carbohydrate consumption
- Exercise intensity
Carbohydrate consumption
When we consume a carbohydrate-rich meal, insulin levels will rise and move the glucose out of the bloodstream and into the cells to be used for energy. At the same time, fat will be ‘spared’ and stored in the adipose tissue.
So, in the hours after a carbohydrate-rich meal – or you eat a high-carbohydrate diet – glucose becomes the primary fuel source for muscles and organs. If we consume a lower-carbohydrate meal, our body switches to burning more fat.
Exercise intensity
Fat is the preferred fuel source for healthy individuals at rest and lower-intensity exercise. Fat is also the primary fuel in lower to medium-intensity exercise, with less glucose being used.
When you perform high-intensity exercise, the body uses more glucose, which becomes the primary fuel.
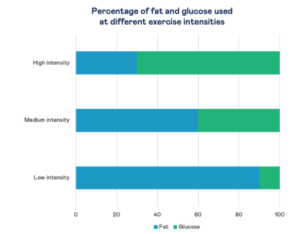
This is because the body can burn glucose at a faster rate compared to fat. When you’re at rest or doing low-intensity exercise such as walking, your body doesn’t require the fast fuel of glucose, so it mainly burns fat.
How is fat utilised for energy?
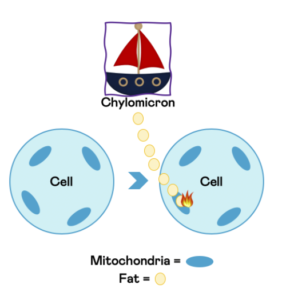
When a cell needs to use fat for energy, such as cells in the muscles or heart, chylomicrons (the boats) will transport fat into the cells to be burnt by what’s known as the mitochondria.
Mitochondria are known as the powerhouses of the cell. It’s here that a cell will take nutrients, such as fat and carbohydrate, and burn them to create energy.
What determines whether fat is used for energy or stored in the adipose tissue?
There are two key factors:
1) Energy balance
When we consume too much energy, our cells (in our muscles, for example) will take in a lot of energy. Too much energy within the cells can be damaging as this can impact their ability to function correctly.
To prevent this, cells will block or slow down the transportation of fat from chylomicrons into the cells around the body. The cells tell the boat that the port is full and to continue its journey.
The chylomicrons transport fat to the adipose tissue to be stored as subcutaneous fat (the fat beneath your skin).
2) Insulin levels
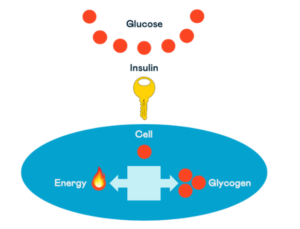
The hormone insulin acts like a key and moves glucose out of the blood and into the cells, but insulin also plays a crucial role in fat regulation.
When insulin levels are high, your body switches to a state of ‘fat storage’. Insulin tells the adipose tissue to store fat, and the body uses more carbohydrates (glucose) for energy instead.
This prevents different body areas from being overrun with energy from both carbohydrates and fat. As mentioned above, this excess energy can be damaging and prevent our body’s cells from functioning correctly.
These two factors are often interlinked. With excess energy storage, you’ll typically see high insulin levels too.
However, you can develop a condition with chronically elevated insulin levels without overconsuming total energy. This condition is known as insulin resistance and can be caused by a diet high in ultra-processed foods that contain refined carbohydrates, sugar, and added vegetable oils.
Key points:
- Fat cells in the adipose tissue can take in excess energy in two ways, by expanding in size or number.
- Fat is utilised in the mitochondria of the cells to be burnt for energy.
- Apart from the brain (which primarily uses glucose for energy), the body’s preferred fuel source will depend on how many carbohydrates you eat and your exercise intensity.
- Excess energy intake and/or high insulin levels determine whether the body will use fat for energy or store it in the adipose tissue.
3) How carbohydrates influence energy use
As mentioned above, the two main factors determining whether fat is stored or used for energy are excess energy intake and insulin levels.
Eating many carbohydrates – particularly refined carbohydrates found in ultra-processed foods – can lead to excess energy intake, high insulin levels, and insulin resistance.
Carbohydrates (glucose) enter the cells from the bloodstream with the support of insulin. Glucose is then used for energy or stored as glycogen for later use.
While we have a large capacity for storing fat in our adipose tissue (a lean adult male will have around 50,000 calories stored), we have a minimal capacity for storing glucose in the form of glycogen (around 1,500 calories in our muscles, 400 calories in our liver).
Imagine you have two suitcases; one is much smaller than the other. The smaller suitcase represents your glycogen stores, so this is where the carbohydrates from the food you’ve eaten get stored if the body does not use them for energy. The larger suitcase represents your fat stores.

When you fill-up your small suitcase by putting too many clothes in, you need to find another place to put the rest. It would make sense that you’d probably put the rest of your clothes in the bigger suitcase.
If it has to, the body will convert the excess glucose into fat to store it in the adipose tissue. It’s transferring energy from one form (carbohydrate) to another (fat).
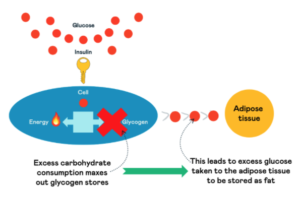
The storage of fat in the adipose tissue (whether it’s from fat or converted from glucose) is a protective mechanism. It prevents excess energy from building up in parts of the body, excess energy from circulating in the bloodstream, and fat build-up in our internal organs.
The importance of healthy adipose tissue
If the ability to store fat in adipose tissue protects our cells and organs, what happens when it can no longer do this?
At this point, fat will start to be stored within the internal organs as visceral fat, and chronic diseases such as type 2 diabetes will start to develop or accelerate.
An example of this is displayed in the image below. Participants A and B have a similar BMI and the same total fat volume stored around their trunk (ASAT + IAAT = total trunk fat).
However, compared to participant A, participant B has a much higher volume of fat stored within the internal organs, called intra-abdominal adipose tissue, and a lower volume of fat stored around the internal organs, called abdominal-subcutaneous adipose tissue (ASAT).
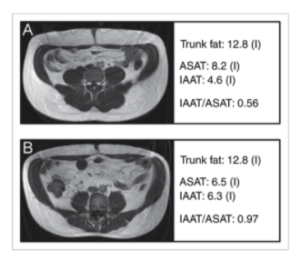
This indicates that participant A has a greater capacity for storing fat in the form of subcutaneous fat in the adipose tissue compared to participant B. And therefore, will have a much lower risk of developing type 2 diabetes.
Key points:
- Consuming excess carbohydrates influences the two main factors leading to fat storage by contributing to excess energy intake and increased insulin levels in the body.
- We have a large capacity for storing fat (50,000+kcal), but we only have a limited capacity for storing carbohydrates as glycogen (~2,000kcal).
- When you’ve reached your glycogen capacity, excess carbohydrates can be converted to fat in the liver or the adipose tissue.
- Storing excess energy beneath our skin in the adipose tissue is a protective mechanism.
- When an individual reaches their personal fat threshold, increased fat levels will be stored in the internal organs.
- This can’t be predicted by BMI or total fat storage (body fat percentage).
- As the volume of fat stored in the organs increases, so will our risk of developing type 2 diabetes and other chronic diseases.
Take home message
The body’s ability to store fat in the adipose tissue as subcutaneous fat is an essential process for ensuring:
- Excess energy doesn’t build up in the cells such as those in the muscles or organs.
- Excess energy doesn’t build up in the bloodstream.
- Fat isn’t stored within the internal organs as visceral fat.
This is the key to understanding the ‘personal fat threshold’ hypothesis.
Our weight or body fat percentage can’t solely predict our risk of developing chronic diseases such as type 2 diabetes. The most crucial factor is where the fat is stored rather than how much.
In part three of this series, we’ll dig into the science of insulin resistance and how this is impacting your risk of type 2 diabetes.


